Note: The definitions of terms marked in (*) are in the glossary at the end of this article.
Adult stem cells are undifferentiated cells in a tissue or organ.
They can renew themselves and differentiate into specialized cell types. They are called into action by normal wear and tear on the body and when severe damage or disease attack.
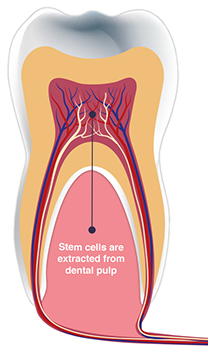
Dental stem cells are located within the pulp (*) of the tooth. Therefore, they are known as DPSC (dental pulp stem cells) or MSC (mesenchymal stem cells). We get DPSC from teeth, but they can differentiate into multiple tissues to help treat medical diseases. The discovery of dental stem cells was in the year 2000, and they are similar to bone marrow stem cells, except they are much easier and less painful to access. There are over 1000 published studies identifying the therapeutic potential of dental stem cells. For example, researchers made insulin (*) and the creation of organs for transplant from mesenchymal stem cells.

The medical future of dental stem cells looks bright and can give our patients “peace of mind” and could potentially cure or save a patient’s life.
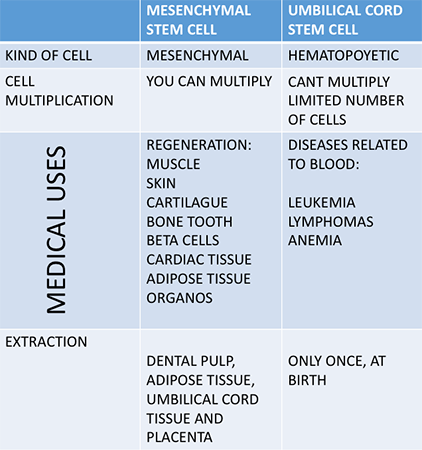
There are advantages of DPSC over those from the umbilical cord:
- You can only use the umbilical cord once to reproduce cells, whereas the stem cells in teeth can be used multiple times and produced faster than any other cells in the body.
- Harvesting DPSC is a minimally invasive process, and the cells the clinician acquires are from teeth we are already removing for other reasons.
- There are no moral, legal, or ethical issues like there are with umbilical cord blood.
- Multiple family members can use the same sample of stem cells.
Umbilical cord stem cells are from different lineage compared to DPSC. Some parents opt to save the umbilical cord stem cells and birth and later obtain the ones from the tooth cells when their child is a young adult. In addition, cord blood stem cells can help rebuild a healthy blood system damaged by disease. DPSCs are not capable of the above.
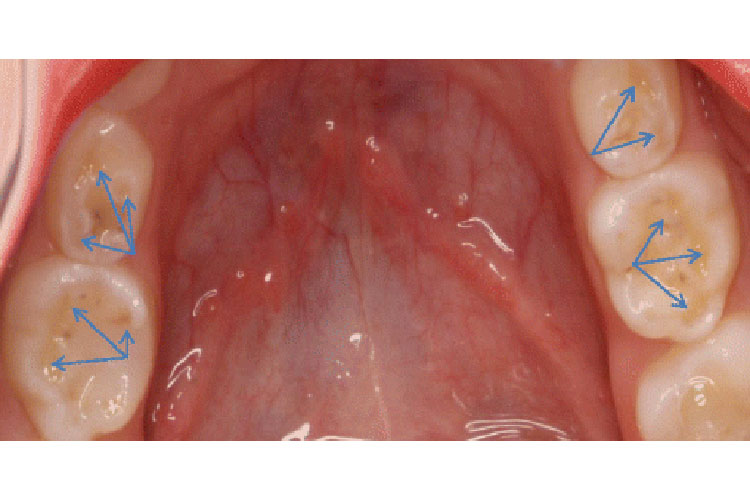
In a young adult, There are about 2-4 million stem cells per impacted wisdom teeth. As time goes on, this number decreases. With age and disease, MSCs predominantly convert into lipid-accumulating fat cells. We take out a lot of 3rd molars, premolars for orthodontic purposes, and primary teeth. Located within the pulps of these teeth are mesenchymal stem cells, which are adult stem cells. The location of the stem cells is also around the dental follicle, periodontal ligament (*), and the apical papilla at the bottom of the tooth root.
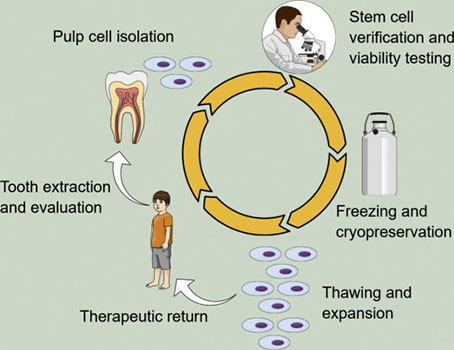
The first part of the process begins in the dental clinic. The patient will consult the dentist and present the option of harvesting stem cells. If the patient/guardian accepts, we place a tooth in a dental stem cell kit that contains Hank’s balanced salt solution (*), which is physiologic. We also place the follicle in the solution if we remove the third molars- as they can also extract stem cells from them. Once they are in the kit, we pack them in a freezer bag with an ice pack; it is fed-ex. Usually, it goes to the company within 24 hours.

The American Association of Tissue Bank regulates all steps involved in stem cell harvesting. For example, after a tooth arrives at a tissue bank lab, disinfection occurs through washing steps using a Listerine-type disinfectant followed by an iodine solution. First, washing removes blood and other pathogens that could contaminate the expansion culture. Next is the tissue extraction process, a precise technique to crack open the tooth and carefully remove the tissue. After removing the tissue from the tooth, it is minced by scalpel blades and digested using a collagen-type (*) solution to break down the tissue into a single-cell solution. After the tissue digestion into a single-cell suspension, the clinician “plates” the cells, and only mesenchymal stem cells stick to the plate. Other cells, like blood, bone, cartilage, muscle, and neuron, remain in the suspension and are washed off with the first media change. Cells are then cultured in mesenchymal stem cell media and allowed to increase. Once a culture is established, the cells double about every two days. It will enable the ability to expand the cell number to achieve a therapeutically relevant number of cells. DPSC storage is at less than 150 degrees Celcius in a cryopreservation process. Facilities use a real-time temperature monitoring system to monitor the temperature in the liquid nitrogen storage tanks.
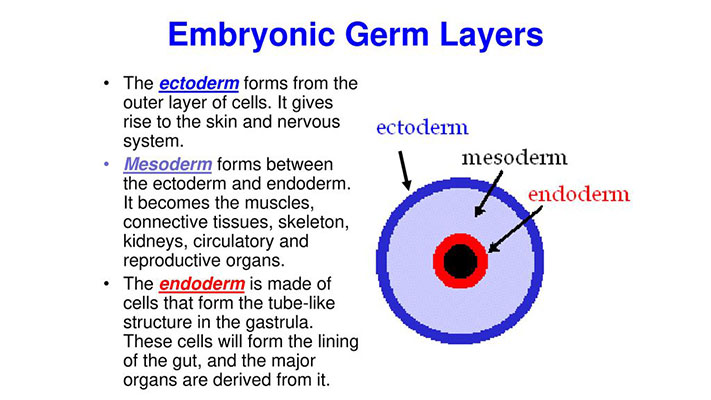
While MSCs come from various sources and can differentiate into multiple tissues, research has shown that the DPSC may be original from the “embryonic ectodermal lineage” (*), which gives rise to the nervous system. The mesenchymal cells can differentiate into bone, cartilage, muscle, marrow, tendons, adipose, and connective tissue.
Any tooth with a viable pulp (must have blood flow) can be a stem cell source even if the tooth has a cavity. Unfortunately, this means you cannot use teeth that have had root canal treatment. However, you could harvest the pulp tissues during endodontic treatment and preserve them at that time. You can use harvest pulp stem cells even if the patient has an infectious disease. In this case, clinicians may only use the cells of the patient from which they are coming. Even if the dentist surgically splits a tooth during its removal., the tissue can still be viable.
There is no restriction age to harvesting DPSC; however, we currently think that most stem cells come from patients under 25. Deciduous teeth are a good source of stem cells, but the number of cells harvested is less than in 3rd molars. The success of your stem cells between relatives decreases depending on the number of generational differences. For example, if your brother used your stem cells, the success rate may be 75%. If your father used them, the success rate might be about 25-50%.
The current research shows that you can take DPS and encourage them to grow into many tissues. The benefits to the patient include:
- Tissue regeneration: the ability to cure gum disease by regenerating healthy gingival tissue.
- Bone regeneration: the ability to grow bone for both tooth regeneration and jaw reconstruction.
- Nerve regeneration: the ability to regrow nerves for multiple applications in dentistry and beyond.
Current stem cell applications in cancers (leukemia and lymphoma), metabolic disorders (*), gum disease, failure diseases, cardiovascular diseases, spinal cord injury, bone and cartilage repair, and multiple sclerosis. Emerging stem cell applications include strokes, type 1 diabetes, brain injury, cerebral palsy, muscular dystrophy, autism, Alzheimer’s, tooth loss, jaw regeneration, facial reconstruction, heart defects, heart and kidney diseases, deafness, and Crohn’s disease.
There is a recorded case of a patient with type 1 diabetes being able to regenerate islet cells of the pancreas (*) with dental pulp stem cells, which allowed them to get off of her insulin. At Columbia University, they have created collagen scaffolding for a tooth. They are experimenting with injecting a stem cell paste into the scaffold. In the future, we may be able to regenerate whole teeth to use instead of dental implants.

In the lab, researchers grew a new tooth for a rat. Two types of mouth stem cells containing genetic instructions for making teeth were mixed and allowed to grow in a lab. After five days, a tooth bud formed. Implantation of the bud into a hole drilled into the mouse’s jawbone followed, and it began to grow. After five weeks, the tip of the tooth started to peak through the gum tissue, and then two weeks later, the mouse had a fully developed tooth. Similarly, a researcher in Tokyo gave grown ear cartilage on the back of a rat. The next step will be transferring this research to humans.
We hope you have enjoyed this article; thank you for reading it!
Glossary of Terms:
- Cell: the smallest functional unit of a living entity, consisting of cytoplasm and organelles enclosed in a membrane.
- The pulp: a mass of connective tissue that resides within the center of the tooth.
- Mesenchymal stem cells (MSCs): are multipotent stem cells found in the dental pulp and bone marrow that are important for making and repairing animal tissues.
- Insulin: A pancreatic hormone generated by the islets of Langerhans, which balance the amount of glucose in the blood. The lack of insulin leads to a form of diabetes.
- Periodontal Ligament: A fibrous joint anchors the tooth’s root to the alveolar bone socket.
- Hanks’ Balanced Salt Solution: A liquid composed of inorganic salts and supplemented with glucose. The solution is to wash cells and maintain cells in a viable state.
- Collagen: The main structural protein found in skin and other connective tissues.
- Ectoderm: is one of the three germ layers made in early embryonic development. It is the source of various tissues and structures (such as the epidermis, the nervous system, and the eyes and ears).
- Germ layer: each of the three layers of cells (ectoderm, mesoderm, and endoderm) that form in the early embryo.
- Embryo: an unborn offspring in the early process of development.
- Metabolic disorder: any of the diseases or disorders that disrupt normal metabolism, the process of converting food to energy on a cellular level.
- Islet Cell: A pancreatic cell that produces hormones (e.g., insulin and glucagon) that are secreted into the bloodstream.
Reference:
Ziauddin, S.M., Nakashima, M., Watanabe, H. et al. Biological characteristics and pulp regeneration potential of stem cells from canine deciduous teeth compared with those of permanent teeth. Stem Cell Res Ther 13, 439 (2022). https://doi.org/10.1186/s13287-022-03124-3
- St. Lawrence Dentistry Looks Forward To St. Patrick’s Day! - March 12, 2025
- Understanding Dental X-Rays and Radiation: What You Should Know - January 13, 2025
- Happy New Year from St. Lawrence Dentistry! - December 30, 2024